Risk factors & symptoms
Poor blood circulation of the legs is caused by the build-up of plaque in the blood vessels (especially the arteries) called atherosclerosis.
Poor Circulation in the Legs? We can help with that!
Poor blood circulation of the legs is caused by the build-up of plaque in the blood vessels (especially the arteries) called atherosclerosis.

Over time, the build-up of plaque in the arteries results in reduced flow of oxygen-rich blood to the tissues. This may result in symptoms of the legs and / or feet including:
More seriously, the build-up of plaque in the arteries may lead to blood clots causing heart attack and / or stroke.
A diagnosis of PAD will require a comprehensive assessment by a medical professional or vascular consultant, and will include a review of medical and family history, a physical examination and referral for relevant diagnostic testing.
The goal of PAD treatment is to improve the blood supply to the legs and therefore reduce symptoms, improve mobility and quality of life, and reduce the risk of serious complications such as heart attack and / or stroke.
The type of treatment required will be based on the medical assessment, though commonly includes lifestyle changes, medication and / or surgery.
Varicose veins are bluish blood vessels, often visible at the back of the knee, or on the lower leg and ankle. They are fairly common and, in the long term, many people will develop them at some point.
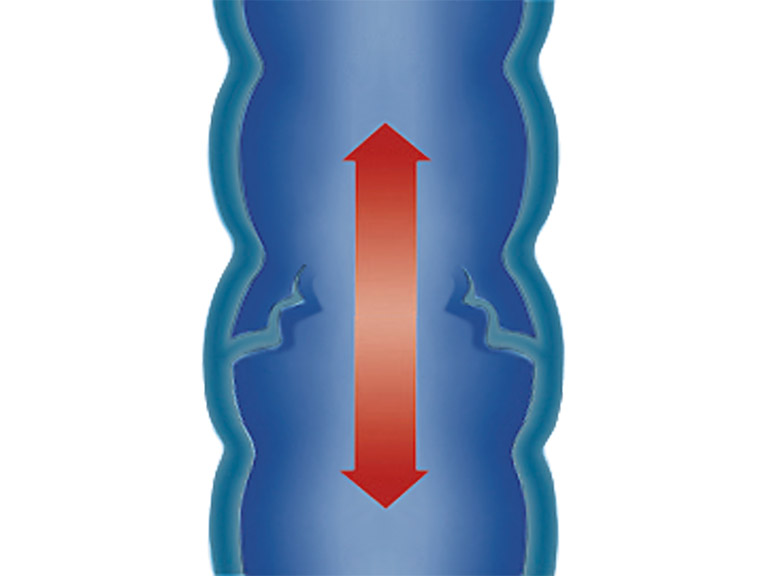
But what are varicose veins precisely? Simply put, they are expanded, swollen and twisted veins in which the venous valves are no longer functioning properly. When standing or sitting, the blood in these pathologically altered veins is no longer transported back rapidly enough to the heart. This results in so-called vascular congestion.
Varicose veins usually don’t constitute a serious medical condition. For many people, they are simply a cosmetic concern, while for other varicose veins cause aching pain and discomfort. Nevertheless, if this venous disease progresses, it can cause much more severe issues like venous leg ulcers.
Varices can lead to symptoms like:
If you are experiencing some of these symptoms and a medical professional recommends treatment, there are a few options available. Compression, for example, is an effective method of relieving the symptoms: at JOBST, we have a range of medical compression stockings specially designed to counteract varicose veins and other venous symptoms. Additionally, exercising regularly and elevating your legs when you sit or lie down is highly beneficial. If you’re still in discomfort, or have any concerns, consult your doctor – they can help you further.
Lymphedema is a term used to describe the accumulation of protein-rich fluid (called lymph) in a particular part of the body, resulting in swelling of the affected area(s). The lymphatic system is made up of a network of lymphatic vessels, lymph nodes and other lymph tissue. It forms part of both the circulatory and immune systems, and is essential for both the transport of lymph and the body’s immune function. Lymphedema occurs either because the lymphatic system isn’t working properly, or there is simply too much fluid for a normal lymphatic system to process.
Traditionally, there are two types of lymphedema, primary and secondary. Primary lymphedema occurs as a result of congenital abnormalities of the lymphatic system. Symptoms may be present from birth or appear later in life. Secondary lymphedema occurs due to damage to a previously intact lymphatic system. A common cause of secondary lymphedema is cancer or its treatment.
Lymphedema is not easy to diagnose because sometimes first symptoms occur after many years. Nevertheless, it is important to get the accurate diagnose and treatment as soon as possible.

Diagnosis of lymphedema requires assessment by a doctor or healthcare professional who has undergone specialist training in lymphedema assessment and its management. Early diagnosis is essential to facilitate timely treatment. Receiving lymphedema risk-reduction education is also important for those at risk of the development of secondary lymphedema.
At Cobblestone Medicine and Rehab Centres, we use both JOBST and Bauerfiend Medical Grade Compression Stockings.



